For more than a decade, studies have sought to address the best treatment strategy for patients with chronic coronary syndromes (CCS), with many suggesting an invasive approach through revascularisation (percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG]), and others suggesting a conservative strategy, such as optimal medical therapy (OMT), for this heterogeneous group of patients.
Two important trials, the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial and the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial, were completed before the routine use of drug-eluting stents (DES) and enhanced adjunctive pharmacotherapy.1,2 The COURAGE trial demonstrated that the addition of PCI to OMT did not reduce the long-term rates of death and non-fatal MI, and the BARI 2D indicated less angina and subsequent coronary revascularisation. A meta-analysis in 2012 involving 7,229 patients did not demonstrate any reduction in death or MI with PCI versus OMT for patients with CCS.3 It is important to mention that, in that meta-analysis, up to one-third of patients in the OMT group required unplanned revascularisation at some point. With the subsequent development and introduction of novel stent technology (i.e. second-generation DES, thinner struts, bioresorbable polymers) and contemporary medical therapy, the need for randomised clinical trials became important.
The recently published International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial was a multicentre randomised trial that commenced in 2012.4 In total, 5,179 patients with moderate to severe ischaemia were assigned to an initial invasive strategy (either PCI or CABG) plus either OMT or a conservative approach, based on OMT alone, with a median follow-up of 3.2 years. The main objective of the ISCHEMIA trial was to determine the effect of adding cardiac catheterisation and revascularisation to OMT in patients with CCS and moderate to severe ischaemia. Ischaemia had to be demonstrated using stress imaging or exercise-stress testing without imaging. High-risk patients were excluded, including those with recent acute coronary syndromes, an estimated glomerular filtration rate <30 ml/min/1.73 m2, an unprotected left main artery stenosis >50% by coronary computed tomographic angiography (CCTA), left ventricular ejection fraction <35%, New York Heart Association class III or IV and unacceptable/persistent angina despite OMT. The primary outcomes were a composite of death from cardiovascular (CV) causes, MI, hospitalisation for unstable angina, heart failure and resuscitated cardiac arrest. Secondary outcomes were a composite of death from CV causes, MI and angina-related quality of life.
The results of the study showed that an initial invasive strategy did not significantly reduce the rates of the primary or key secondary composite outcomes among patients with CCS and moderate to severe ischaemia upon stress testing. These results are in accordance with previous evidence, and although it would be easy to generalise these assumptions and continue to reduce the volume of PCIs performed in CCS patients, the incidence of MI in this landmark clinical trial needs to be discussed.5
MI in both groups demonstrated a particular behaviour. Patients in the invasive strategy group had a higher rate of non-significant CV events (CV death/MI) during the first year of follow-up due to an increased incidence of procedural MI. However, patients in the conservative strategy group had a higher rate of non-significant late CV events due to an increased incidence of non-procedural MI. Although the incidence of procedural MI was higher when the secondary MI definition was used, the opposing trend in MI was the same regardless of the definition.
We know from previous studies that procedural MI are associated with an increased risk of morbidity and mortality during the first year after revascularisation, and this clearly explains the higher incidence of early events in the invasive strategy group.6–8 As there is a lack of information relating to specific invasive percutaneous and surgical procedures, such as anatomical complexity, risk stratification, procedural success rate, stent restenosis/thrombosis, the incidence of chronic total occlusion, number of grafts, cardiopulmonary bypass time and complications, among many others (most of which are known procedural MI risk factors), it is futile to try to interpret the relevance of early procedural MI within the invasive strategy group.9 Instead, we focus on late CV events driven by differences in non-procedural MI between both treatment strategy groups.
After the second year, the conservative strategy group had a higher, sustained increase in the incidence of non-procedural MI compared with the invasive strategy group. Interestingly, this did not translate into increased mortality. One-fifth of these patients underwent revascularisation at some point during follow-up; 30% due to a confirmed primary event and 69% due to a suspected primary event, refractory angina, non-adherence or other event. Although differences in both early and late events lacked statistical significance, there was a clear separation in the time-to-event curves of non-procedural MI towards the end of the clinical follow-up period. This finding should compel researchers to undertake a longer monitoring period to establish if there are further differences in non-procedural MI rates, as a preliminary analysis of the ISCHEMIA trial data showed that non-procedural MI resulted in a higher risk of subsequent death when compared to procedural MI. Furthermore, a recent meta-analysis of more than 14,000 patients (including ISCHEMIA patients) showed a significant decrease in late non-procedural MI with revascularisation at the expense of an increase in early procedural MI, indicating the benefits of revascularisation in CCS.10
There are some factors that we think could have influenced the incidence of late events in the invasive group. First, almost half of the randomised patients had angiographic or tomographic evidence of three-vessel disease. We know from previous studies that, in multivessel disease, single-photon emission computed tomography underestimates the true extent of coronary artery disease.11 Therefore, this poses the question of how many patients with mild/moderate ischaemia had the degree of their defect underestimated, and subsequently had a misled revascularisation. These non-obstructive lesions with mild/moderate ischaemia that were not revascularised could in part be responsible for late CV events.
Second, as part of the study protocol, vessels with stenotic lesions between 50% and 79%, with no ischaemia observed on stress imaging in the distribution of the stenosis, were required to have fractional flow reserve (FFR)/instantaneous wave-free ratio (iFR) performed to proceed with PCI. Despite this, the reported use of FFR/iFR was roughly 20%. PCIs for these types of lesions and the use of intravascular physiology were left to the operator’s discretion. As such, we question whether a stricter application of FFR/iFR could have led to a decrease in the rates of urgent revascularisation, as previously reported.12 Also, intracoronary physiology could have been very useful in patients with severe diffuse ischaemia without significant coronary stenosis.
Third, we question whether vulnerable non-obstructive plaques could be responsible for late non-procedural MI in the invasive strategy group. Recent evidence has shown that near-infrared spectroscopy ultrasound imaging can evaluate vulnerable plaques and identify segments and lesions at risk of future coronary events.13 To date, there has been no robust data that stenting non-obstructive vulnerable plaques leads to better clinical outcomes, although it has been reported that stenting significant vulnerable plaques does.
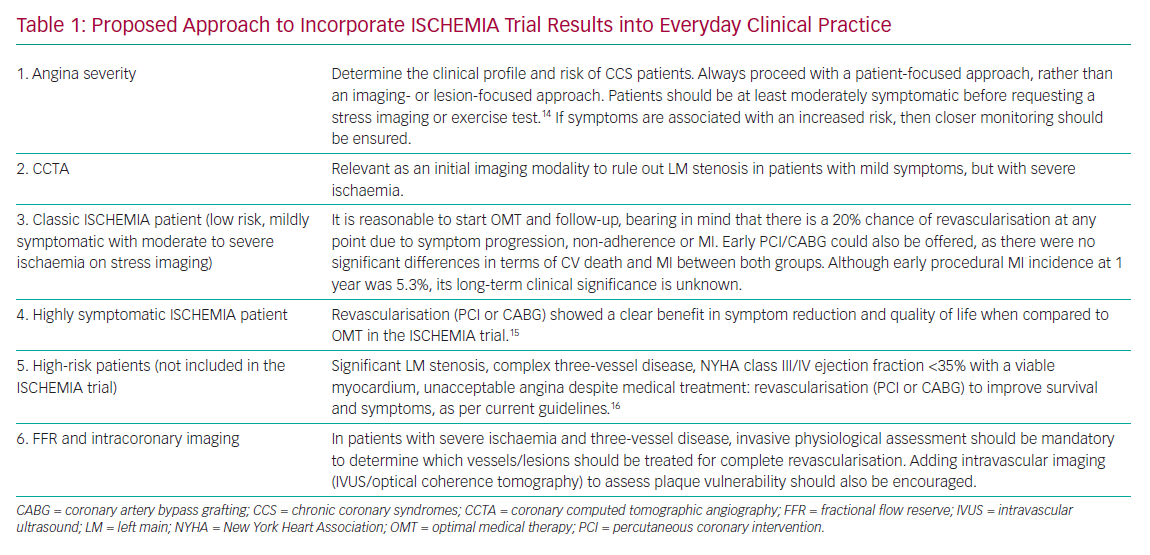
The results presented in this remarkable landmark trial provide us with valuable information and lessons that can be incorporated into daily practice (Table 1).
From a methodological point of view, there are some considerations that may be of great interest and warrant further investigation. First, the primary outcome definition was modified throughout the study as a protocol-defined procedure due to slow recruitment and lower-than-expected aggregated event rates. The reduction in sample size then resulted in a decrease of power.
Second, the follow-up, as stated by the authors, was modest, with a 3.2-year median follow-up period. In terms of MI, there was a continuous and sustained, although non-significant, separation of the curves after the third year, with a greater number of non-procedural MIs in the conservative group. As previously discussed, a longer follow-up period is mandatory and will help to clarify whether the lack of differences in the primary outcomes between the groups is maintained over time.
Third, it is important to point out that, even though a secondary MI definition was added at some point during the study, this did not impact the results. Procedural MIs were more prevalent in the invasive group, and non-procedural MIs were more prevalent in the conservative group, regardless of the definition used.
Fourth, the majority of randomised patients were either asymptomatic or mildly symptomatic, so we must be cautious and avoid extrapolating these results to a more symptomatic/higher-risk group of patients.
Fifth, from an anatomical point of view, in the setting of moderate to severe ischaemia, the proportion between one–two vessel disease and three-vessel disease was about equal, which is remarkable. Anatomical complexity, employing the SYNTAX score, was not reported.
Sixth, PCI and CABG were treated as equivalent methods of revascularisation in the invasive group. Future analyses by the authors will clarify whether there is a difference in mortality and MI between these two revascularisation modalities in the setting of CCS. As per protocol, patients with a low SYNTAX score were deemed suitable for PCI, whereas patients with a high SYNTAX score were treated with CABG. Patients with an intermediate SYNTAX score could have either based on the centre of practice. Given that almost 75% of patients in the invasive group were treated by PCI, we can imply that the majority had low/intermediate anatomical complexity. This supports the concept of an ISCHEMIA type of patient being of low/intermediate risk, mildly symptomatic with moderate to severe ischaemia and with low/intermediate anatomical complexity.
Finally, in the statistical analysis, the proportional hazards assumption underlying the Cox model was not met for the primary outcomes (patients in the invasive group had an increased risk of having a procedural MI, whereas patients in the conservative group did not). Given this proportional hazards assumption violation, secondary outcomes were reported as cumulative event-rate estimates with CIs, which underpowers the conclusions and makes them difficult to interpret.
Conclusion
The available data from randomised trials, including the ISCHEMIA trial, provide enough evidence to implement an initial OMT strategy in mildly symptomatic, low-risk patients, regardless of the degree of ischaemia on stress or exercise imaging. Around 20%–30% of these patients will require either a PCI or CABG due to angina progression/unresponsiveness to medical therapy, non-adherence or development of an acute coronary syndrome. The invasive strategy showed a non-significant lower incidence of late non-procedural MI at the expense of early procedural-MI, so follow-up for ISCHEMIA trial patients should continue, because there could be greater differences in the rate of non-procedural MI over time. These results should not be extrapolated to a more symptomatic, higher-risk population, as this specific niche of patients was not included in the study.
Decision-making processes in these heterogeneous stable coronary disease patients should continue to be individualised, taking into account risk factors, symptoms, medical therapy adherence, procedural risks and the patient’s preference. We recommend a patient-centred approach, rather than an imaging or lesion-centred approach, to determine the best treatment strategy.
It is important that trials that include patients with frequent angina and proven severe ischaemia with the routine use of coronary physiological assessment and coronary imaging are conducted as soon as possible. This will undoubtedly help to clarify most of the ambiguities in the current results.