Intracoronary measurement of myocardial FFR is a simple, reliable and reproducible index of the physiological significance of coronary stenosis. In addition, FFR assessment can be used to guide PCI, improving procedural outcomes. However the impact of FFR values after PCI on clinical outcomes remains unclear.
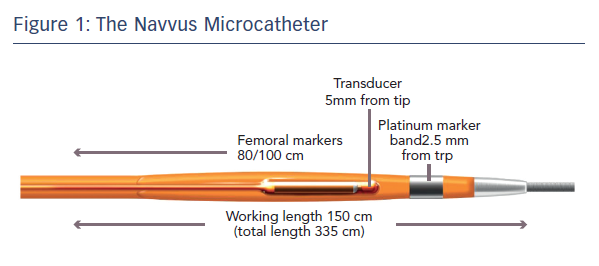
The FFR-SEARCH study aimed to determine the impact of post-PCI FFR values on long-term clinical outcomes in a prospective all-comer registry study.9 All patients who underwent successful PCI were eligible. An FFR assessment using the ACIST RXi system and Navvus microcatheter was performed after each PCI when the angiographic result was considered acceptable by the operator. Wire access to the vessel was maintained and a pressure sensor FFR microcatheter was inserted over the previously used coronary guide-wire. The Navvus microcatheter allows FFR assessment after crossing the lesion with any 0.014" guidewire of choice. A platinum marker band is located 2.5 mm from the tip and a fibre-optic sensor 2.5 mm from the marker band (5 mm from the tip).7 This gives a profile comparable to 0.022" diameter at the lesion site (see Figure 1).
The study screened 1,512 patients undergoing PCI. Of these, 512 patients were excluded: 156 because of unstable disease, 148 because of operator decision, 129 because vessels were too small and 79 for other reasons. Of the 1,000 patients who underwent assessment using the Navvus microcatheter, the wire did not cross the lesion in 28 cases, equipment failure occurred in 11 cases and two patients had an adverse response to adenosine. Of the remaining patients, 1,165 lesions had a successful post-PCI FFR measurement. Failure to cross the lesion was reported in 14 procedures, nine patients were not assessed because of unstable disease, 22 lesions were not measured because of operator decision and 28 for other reasons. In 109 lesions the vessel was too small and there was one case of equipment failure. The baseline characteristics were reported on 1000 patients and procedural results were reported on 959 patients with 1,165 lesions. The average age at baseline was 64.6 ± 11.8 years and patients were predominantly male (72.5 %). Of note, clinical presentations were evenly distributed between stable angina (30.4 %), unstable angina/non ST-elevation MI (36.7 %) and acute MI (32.9 %), i.e. >60 % of the patients involved were unstable.
Where possible, FFR was performed at least 20 mm from the most distal stent then a pullback was performed to obtain pressure gradients on the distal and proximal stent edge border as well as to assess overall drift at the ostium. The average drift value was low, 0.011 ± 0.015, and the average procedural time per lesion was 5.0 ± 1.4 minutes, which included the full duration of the adenosine infusion, showing that FFR can be used quickly to evaluate PCI results. Failure to cross the post-PCI lesion occurred in 42 of 1,207 (3.5 %) attempted lesions, mostly because of tortuosity and calcification, and there were no Navvus-related complications reported.
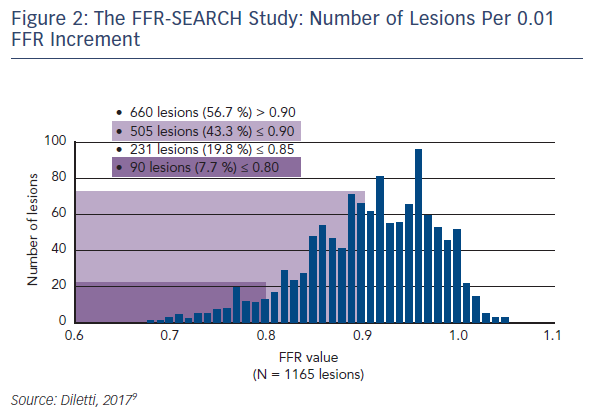
Dr Diletti presented preliminary outcome data from this study. Patientlevel analysis showed that almost half (48 %) of patients had an FFR below 0.90. Lesion level assessment showed that in 43.3 % of cases, the FFR was ≤0.90. In 7.7 % of lesions post-stenting FFR was below the threshold for ischaemia (i.e. ≤0.80). The number of lesions per 0.01 FFR increment was 660 lesions (57 %) with FFR >0.90; 505 lesions (43 %) ≤0.90; 231 lesions (20 %) ≤0.85 and 90 lesions (8 %) ≤0.80 (see Figure 2). The cut-off of 0.90 could help guide procedural optimisation.
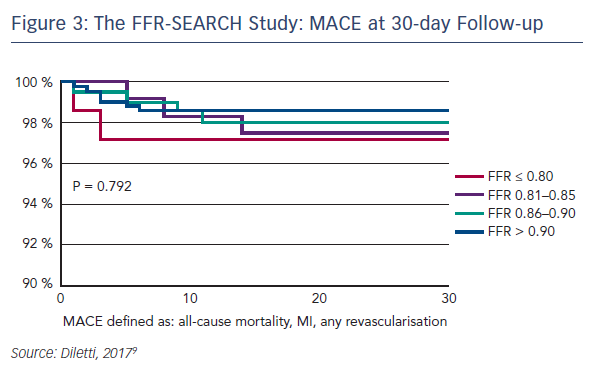
The primary outcome measure was major adverse coronary events (MACE), including all-cause mortality, Q-wave MI, target lesion revascularisation, target vessel revascularisation, stent thrombosis and any revascularisation at 30 days. Of 798 (89 %) patients with complete 30-day follow-up, MACE occurred in only 15 (1.9 %). The MACE rate for each subgroup at 30 days did not differ significantly between groups: FFR ≤0.80 2.8 %, FFR 0.81–0.85 2.6 %, FFR 0.86–0.90 2.0 % and FFR >0.90 1.5 % (see Figure 3). Although not statistically significant, it is interesting to observe the initial trend of the lower the post-PCI FFR value, the higher the reported MACE rate at 30 days. The study design intended to provide a clear message of clinical outcomes at 2 years.
Dr Diletti summarised the key points of the presentation as follows:
- Microcatheter-based FFR post-PCI allows a safe and rapid physiological assessment of the treatment result.
- A relevant percentage of the stented vessels have a final FFR <0.90.
- PCI optimisation by microcatheter-based FFR may improve clinical outcome.
In the subsequent audience discussion, some experts at EuroPCR questioned whether the FFR was detecting suboptimal stent placement, or if other factors such as microcirculatory problems might be contributing. Others questioned the next step to optimising procedures. The upcoming FFR REACT randomised study aims to evaluate the clinical impact of intravascular-ultrasound-directed FFR optimisation of PCI.