Dr O’Neill stated the causes of cardiogenic shock (CS) that ultimately influence patient outcomes. One of the main causes of significant variation in outcomes when comparing large retrospective registries of CS is the inclusion of patients with CS following an out-of-hospital cardiac arrest (OHCA). Typically, CS after OHCA is mostly due to arrhythmia rather than ischaemia, and these patients may also have neurological injury, leading to a worse prognosis. He emphasised that the National Cardiogenic Shock Initiative (NCSI) is a standardised protocol-based approach to treat CS due to acute MI (AMICS).
Dr O’Neill further highlighted that there are no Class Ia indicated therapy for AMICS in the European Society of Cardiology 2017 guidelines. Randomised controlled trials (RCTs) are challenging in AMICS, particularly in the US, given the need to obtain informed consent. A few RCTs have been conducted in Germany, where there is a system of prospective conditional approval. Therefore, in 2016, Dr O’Neill and colleagues designed a prospective registry to assess outcomes in patients with AMICS treated with Impella based on a standardised protocol. The protocol emphasises the early initiation of Impella support prior to reperfusion in patients with AMICS.
An analysis of data from more than 15,000 AMICS patients treated with Impella in the Abiomed Impella Quality (IQ) registry suggested a wide variation in survival outcomes across centres, based on the volume of Impella use.1 Further analysis of the IQ registry identified three best practices associated with improved survival in AMICS: initiation of Impella support prior to percutaneous coronary intervention (PCI), haemodynamic monitoring using pulmonary artery catheter and the use of Impella CP. Dr O’Neill was excited about the increased adoption of these best practices over time, which was associated with a parallel increase in survival to Impella explantation from 51% in January 2009–December 2016 to 63% in April 2015–September 2018 (p<0.00001). The number of hospital sites in the registry that demonstrated a survival to explantation of >80% increased from 11% in January 2009–December 2016 to 19% in April 2015–September 2018.
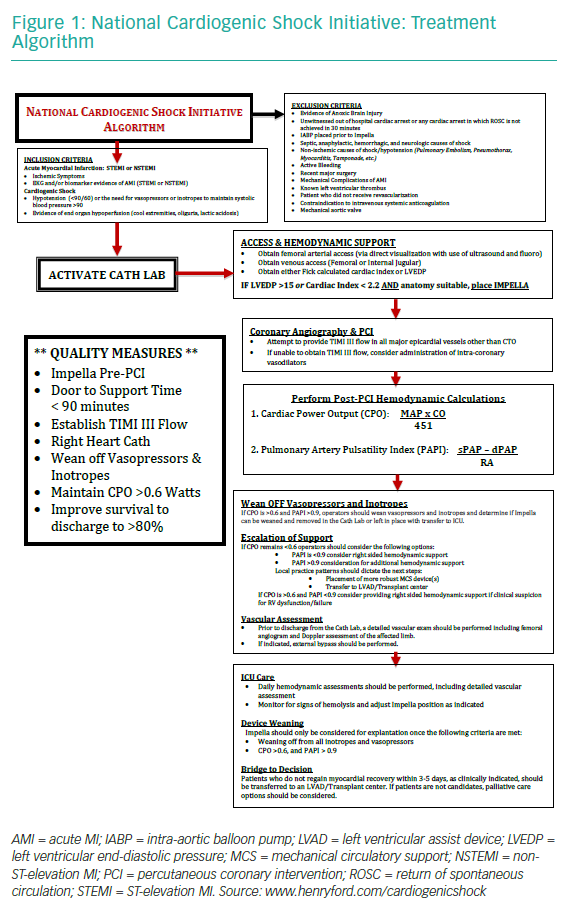
The Detroit Cardiogenic Shock Initiative started in 2016 as a pilot study, with four Detroit sites agreeing to treat all patients with AMICS using a mutually agreed-upon, best-practice algorithm.2 Of the 66 screened patients, 50 were included in the single-arm, prospective, multicentre study. The survival rate was 76%, compared with 53% in the Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock (SHOCK) trial and 53% in the IMPella versus IABP Reduces mortality in STEMI patients treated with primary PCI in Severe cardiogenic SHOCK (IMPRESS in Severe Shock) trial.3,4 The initiative has continued to grow. At present, more than 65 sites around the country are using the algorithm (Figure 1) and best practices, now referred to as the NCSI (NCT03677180).
As of 14 June 2019, a total of 423 patients had been screened for inclusion, of whom 214 were included in the initiative. A recent analysis of 171 patients included in the NCSI (lactate of 5.3 mmol/l and cardiac arrest in 42%) reported the survival rate of 72%.5 This survival rate is higher compared to the SHOCK trial (53%) and Intraaortic Balloon Pump in Cardiogenic Shock (IABP-SHOCK) trial (60%).3,6
Dr O’Neill highlighted that the clinical sites in the NCSI are a combination of academic (38%) and community hospitals (62%). It is important to include community hospitals because 60% of CS patients present to a community hospital. He also emphasised the vital role of the ‘hub and spoke’ model to ensure prompt care for a wide range of patients.
The revascularisation strategy among patients enrolled in the NCSI was analysed. The survival among patients with one-, two- and three-vessel disease treated with a single vessel PCI was 71%, 72% and 75%, respectively. Interestingly, the survival was not significantly different among patients treated with a single-vessel or multivessel PCI, suggesting that the revascularisation strategy does not impact survival rates in this patient population. A potential reason for this effect could be a lower incidence of contrast-induced renal dysfunction in patients supported with Impella. In contrast, >70% of patients in the Culprit Lesion Only PCI Versus Multivessel PCI in Cardiogenic Shock (CULPRIT-SHOCK) trial did not receive haemodynamic support, which is the likely cause of the different outcomes.7 In light of the above findings, Dr O’Neill suggested that the revascularisation strategy in patients with AMICS receiving haemodynamic support needs to be revisited.
Next, an attempt was made to identify important clinical and haemodynamic variables that aid in predicting outcomes post-PCI. Cardiac power output (CPO), cardiac output, cardiac index, pulmonary artery oxygen saturation, pulmonary artery pulsatility index, hepatic enzymes and lactate were found to be useful predictors of survival.5
Stratifying patients according to CPO (> or <0.6 W) and lactate (> or <4 mg/dl) at 12–24 hours post-PCI and Impella support provides a reliable and useful tool for predicting outcomes and the need for escalation of therapy. In addition, survival was lowest for patients with CPO ≤0.6 W and receiving ≥2 inotropes, while highest for patients with CPO ≥0.6 W and receiving 0–1 inotropes post-Impella and PCI.
In conclusion, the findings from the NCSI have demonstrated that a protocol-based approach emphasising best practices is reproducible in institutions across the country in both academic and community programmes and is associated with significant improvement in survival in AMICS compared to historical controls. Future studies will focus on identifying factors that will improve survival to >80% in AMICS.